Developed from British Obesity and Metabolic Surgery Society (BOMSS) Nutritional Guidance Update 2020 by the working group: Dr Helen Parretti, Mary O’Kane RD, Dr Carly Hughes, Sally Abbott RD, Dr Karen Coulman RD, Dr Ruth Mears, Dr Manisha Sharma with input from Dr Emma Shuttlewood.
This document is freely available for clinical use. To use for other purposes, please contact BOMSS at info@bomss.org.
Download this information as a PDF here: BOMSS Post-Bariatric Surgery Nutritional Guidance for GPs
Introduction
This guidance aims to provide GPs with an accessible summary of BOMSS nutritional guidance to support GPs managing adults who have had bariatric surgery.
Please note that this guidance does not replace obtaining clinical support and advice from a bariatric surgery unit and we would always advise seeking help from your local unit or the unit where the patient had their procedure if possible.
Take extra caution with patients who have had surgery abroad as procedures may not be aligned with those performed in the UK.
The focus of this guidance covers only nutritional aspects of follow-up care for adults as recommended by NICE CG189 for NHS patients ≥ 2 years post-surgery. It does not constitute guidance on how to conduct all other aspects (medical, psychological) of a complete annual review post-bariatric surgery. However, guidance for GPs on other aspects of annual reviews is also available on BOMSS webpages together with some links to useful patient support resources.
This guidance does not cover the following patient groups/procedures who need to remain under the specialist care of the bariatric surgery team:
- adolescents
- malabsorptive procedures such as (but not limited to):
-
- biliopancreatic diversion/duodenal switch (BPD/DS)
- single anastomosis duodenal ileal bypass (SADI)
- one anastomosis gastric bypass (OAGB or mini gastric bypass) or any other gastric bypass with bilio-pancreatic limb >150 cm
- Single anastomosis stomach ileal bypass (SASI)
-
Annual blood monitoring and lifelong nutritional supplementation
Following bariatric surgery, patients are at a greater risk of nutritional deficiencies and require annual nutritional monitoring and routine nutritional supplements. These should be continued for life and are summarised in the Tables 1 and 2 below.
Note:
There are a wide range of multivitamin and mineral supplements available over the counter (OTC). Unfortunately, their composition varies widely, and they rarely contain sufficient zinc and copper as recommended in the BOMSS guidelines.
We recommend the multivitamin and mineral supplement is complete and contains a minimum of 400 to 800 micrograms folic acid, 15 mg zinc and 2 mg copper. Consequently, many OTC supplements will have to be doubled to meet these. Forceval is the only vitamin and mineral supplement available on prescription that meets these requirements (correct as of 23.01.23).
Table 1: Routine annual blood monitoring
| LAGB | SG/RYGB, or an OAGB with a BP limb of 150cm or less |
|
|---|---|---|
| FBC | ✓ | ✓ |
| Corrected Calcium (bone profile if not available) | ✓ | ✓ |
| LFTs | ✓ | ✓ |
| U+Es | ✓ | ✓ |
| Vitamin B12 + Folate | ✓ | ✓ |
| Ferritin* | ✓ | ✓ |
| HbA1c, lipids | C | C |
| Vitamin D | ✓ | ✓ |
| Zinc** | S | ✓ |
| Copper** | S | ✓ |
| Selenium** | S | ✓ |
| Vitamins E, A or K1 | S | S |
| C = co-morbidity monitoring if had pre-op diagnosis S = if symptomatic of deficiency (see signs/symptoms table below) *Low ferritin suggests iron deficiency, but a high ferritin level does not rule out iron deficiency (for example, inflammation may raise ferritin levels). A complete iron profile is more useful in this situation. **Note: a trace element vacutainer tube is needed for zinc, copper and selenium tests |
||
Table 2: Routine lifelong nutritional supplements in absence of any nutritional deficiencies
| LAGB | SG/RYGB, or an OAGB with a BP limb of 150cm or less |
|
|---|---|---|
| A-Z Multivitamin and Mineral | ||
| Forceval 1 tablet or OD or equivalent | ✓ | ✓ |
| Calcium and Vitamin D* | ||
| Adcal D3 chewable tablet BD or equivalent (eg. calcium citrate) | ✓ | |
| Iron** | ||
| Ferrous sulphate 200mg OD OR Ferrous fumarate 210mg OD OR Ferrous gluconate 300mg BD | ✓ | |
| Vitamin B12 | ||
| IM vitamin B12 injection every 3 months (even with normal/high levels to prevent deficiency developing) | ✓ | |
| * Patients may need additional vitamin D supplements to reach serum 25 hydroxyvitamin D3 levels ≥ 75nmol/L (monitor and prescribe additional vitamin D supplements alone rather than prescribing additional Adcal D3 (or equivalent)). Calcium citrate is preferred over calcium carbonate in patients with past or family history of kidney stones. ** Iron supplementation needs to be assessed in line with blood test results and additional supplementation may be required. Menstruating women need higher doses: 200mg ferrous sulphate or 210mg ferrous fumarate or 300mg ferrous gluconate tablet twice daily. Note: consider advising iron and calcium supplements to be taken at least 2 hours apart. Iron supplements should be taken with food, while tea/coffee should be spaced at least 90 minutes away from them to allow adequate iron absorption. Some patients especially those with haemorrhoids and history of severe constipation with oral iron supplements might require parenteral iron supplements as and when required. Check formulations for all supplements as these may be changed by the manufacturers over time. | ||
| LAGB=laparoscopic gastric banding, SG=sleeve gastrectomy, RYGB=Roux-en-Y gastric bypass, OAGB=one- anastomosis gastric bypass, BP=bilio-pancreatic | ||
Signs/symptoms of possible nutritional issues post-bariatric surgery (A to Z)
Some key points:
- If patients have one deficiency, they often have others, so it is recommended that if one is identified full screening bloods are requested.
- Vitamin B12 deficiencies may present several years post-surgery.
-
- Serum vitamin B12 levels are not a good indicator of vitamin B12 sufficiency, leading to a significant number of cases of vitamin B12 deficiency not being detected. Some labs can provide serum active B12 (Holotranscobalamine) and serum MMA (Methylmelanoic acid) levels which give a more accurate indication of vitamin B12 deficiency.
- Asymptomatic patients receiving regular vitamin B12 injections every 3 months, do not require serum vitamin B12 testing unless clinically indicated. However, patients symptomatic of vitamin B12 deficiency (neurological features can precede any haematological features) should be referred to a specialist bariatric unit in secondary care for further evaluation and management.
- If serum levels are tested and found to be normal/high continue vitamin B12 injections 3 monthly to avoid future deficiency (serum level must be checked just prior to the next due vitamin B12 injection). However, these serum levels will also need to be clinically correlated and if indicated, the patient referred to an appropriate specialist to rule out a hepatic or myeloproliferative condition as a cause of persistent vitamin B12 deficiency.
-
- Copper/zinc supplementation
-
- Check which vitamin and mineral supplements (prescribed and over the counter) the person is taking. Some people may have stopped taking their supplements or may be taking ones containing high doses of zinc or copper (zinc:copper ratio in supplementation should be 8-15mg:1mg (minimum 2mg copper))
- During acute infection /high CRP, zinc level can drop – avoid supplementing zinc in this scenario. Diagnose and treat zinc deficiency only when established with a normal CRP level.
- For patients with borderline low zinc or copper levels, consider prescribing two Forceval/day to maintain the correct ratio of zinc to copper. Recheck levels after three months.
- For severe zinc deficiency, with normal copper levels, treat with high dose zinc supplement for 3 months and recheck zinc and copper levels. If additional zinc or copper supplements are needed, both should be monitored as they share a reciprocal relationship. High doses of zinc may cause copper deficiency and vice versa. If no improvement or if there is a drop in copper levels, refer back to the bariatric unit. For severe copper deficiency, refer back to the bariatric unit.
-
- Vomiting, dysphagia or regurgitation are not normal consequences of bariatric surgery, and should always be investigated and may occur with any procedure
-
- If a patient eats too fast, the wrong texture of food, or too much, they may experience regurgitation. If this happens frequently it can be a sign of an overtight band or a stricture.
- Patients who present with prolonged vomiting should be referred to a bariatric surgery unit and are at risk of thiamine deficiency. Risk of thiamine deficiency increases with poor nutritional intake, fast weight loss, dysphagia or an inability to meet thiamine requirements through oral diet or supplements. Thiamine deficiency can develop acutely within 9 to 18 days, leading to irreversible neuropathy, Beriberi or Wernicke-Korsakoff syndrome. If there is any suspicion of risk, initiate treatment immediately: prescribe oral thiamine 200–300 mg daily, vitamin B co-strong 1 or 2 tablets, three times a day. Give parenteral thiamine if oral thiamine is not tolerated. If there are suspected neurological complications of thiamine deficiency patients should have a same day referral to the medical team and urgent review by neurology as well as an urgent referral to the bariatric surgery unit.
-
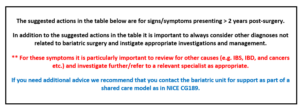
Table 3: Signs/symptoms of possible nutritional issues post-bariatric surgery (A-Z)
| Sign/symptom | Potential cause related to bariatric surgery and nutrients to check | Suggested actions |
|---|---|---|
| Anaemia (symptoms of)** | Iron deficiency, copper deficiency, vitamin B12 deficiency, folate deficiency. | For iron, vitamin B12 or folate deficiencies, manage as per BNF. NICE guidance on folate and vitamin B12 deficiencies can be found here and on iron deficiency anaemia here. For copper deficiency, see notes above this table and refer to bariatric surgery unit for advice. |
| Blood disorders such as thrombocytopenia, leucopenia | Copper deficiency. | Ensure both copper and zinc have been checked. See notes above this table and refer to bariatric surgery unit for advice, and if appropriate to haematology. |
| Cardiomyopathy, unexplained cardiac symptoms | Selenium deficiency and vitamin B12 deficiency. | Refer to cardiology and highlight the history of bariatric surgery. |
| Confusion (unexplained by routine check ups) | Thiamine deficiency, vitamin B12 deficiency. | Refer to medical/neurology team as appropriate. |
| Constipation** | Often the result of a low fibre and / or insufficient fluid intake. | Give advice on dietary sources of fibre and increased fluid intake, laxatives may be required. May be due to an overtight band and patient is unable to manage adequate fluid and fibre intake, in which case refer back to bariatric surgery unit. |
| Diarrhoea** | Diarrhoea and steatorrhoea may occur after gastric bypass, for example this can be caused by small intestinal bacterial overgrowth. | Recalcitrant diarrhoea should be investigated as can contribute to protein malabsorption and vitamin and mineral deficiencies, refer to bariatric surgery unit. |
| Glossitis | Zinc deficiency, iron deficiency. | For iron deficiency manage as per BNF. NICE guidance on iron deficiency anaemia can be found here. For zinc deficiency see notes above this table and refer to bariatric surgery unit for advice. |
| Hair loss | Zinc deficiency, iron deficiency, poor protein intake. | Obtain a detailed nutritional assessment to exclude/identify causes. For iron deficiency manage as per BNF. NICE guidance on iron deficiency anaemia can be found here. For zinc deficiency see notes above this table and refer to bariatric surgery unit for advice. For concerns about protein intake, refer to community dietitian for assessment and review. |
| Hypoglycaemia (symptoms of) after eating (sweating, shaking, feeing unwell, blackouts) | Post Prandial Hypoglycaemia (PPH) - most often seen following a gastric bypass (however it may occur with other procedures). | Referral to a bariatric surgery unit dietetics initially (urgency depends on severity of the symptoms). If dietary education fails to resolve the symptoms, refer for further investigation by a bariatric physician or endocrinologist (urgency depends on severity of the symptoms). |
| Metabolic bone disease | Calcium deficiency, vitamin D deficiency, selenium deficiency. | For vitamin D deficiency, check PTH as it can cause secondary hyperparathyroidism. Follow NOGG guidance. If poor response to vitamin D supplementation, refer to bone clinic. |
| Memory issues | Vitamin B12 deficiency, iron deficiency, thiamine deficiency. | Treat any relevant nutritional deficiencies and if symptoms persist, refer to neurology. |
| Neuropathy/ neuromuscular disorders | Folate deficiency (can cause indirect cellular thiamine deficiency as well), vitamin B12 deficiency, copper deficiency, thiamine deficiency. | For folate and/or vitamin B12 deficiencies manage as per BNF. NICE guidance on folate and vitamin B12 can also be found here. Consider referral to neurology if symptomatic. For copper or thiamine deficiency see notes above this table and refer to bariatric surgery unit for advice. |
| Night blindness | Vitamin A deficiency (for example, after gastric bypass). | If suspected refer urgently to bariatric surgery unit for vitamin A blood test and advise the patient to get a routine eye test conducted by an optician. |
| Peripheral oedema | Protein malnutrition. | Refer to bariatric surgery unit as requires further investigation. |
| Poor wound healing | Zinc deficiency, copper deficiency, iron deficiency, protein malnutrition. | For iron deficiency manage as per BNF. NICE guidance on iron deficiency anaemia is available here. For zinc and/or copper deficiency, see notes above this table and refer to bariatric surgery unit for advice. For protein malnutrition, refer to bariatric surgery unit as requires further investigation. |
| Pregnancy (1,2) | Women are advised to avoid getting pregnant until around 12 to 18 months after bariatric surgery. Preconception planning is important. | Recommend that women have 5 mg/day folic acid, starting before conception and continuing for the first trimester. Vitamin supplements containing vitamin A in the retinol form should be avoided, however, vitamin A in the beta carotene form (e.g. Forceval capsules (BUT NOT the soluble form)) are acceptable (correct as of 23.01.23). Women who become pregnant post-bariatric surgery need urgent referral for consultant-led care. |
| Weight loss (excessive) ** | Multiple potential causes - greatly reduced appetite, inadequate intake, malabsorption, stricture, overtight band, psychological factors including fear of weight gain or diet progression. | Patients with continued, excessive, weight loss require further investigations and referral back to bariatric surgery unit. |
© BOMSS and the authors 2023
